Abstract
Introduction: Sickle cell disease (SCD) is characterized by elevated markers of hemostatic activation and thrombophilia manifesting as arterial stroke and venous thromboembolism (VTE). Anticoagulation for VTE in SCD is associated with an increased risk for bleeding. In cancer patients at high risk for VTE, the flavonoid Isoquercetin (IQ) lowered D-dimer and soluble P-selectin possibly by inhibiting plasma protein disulfide isomerase. In a murine model of SCD, IQ with Hydroxyurea (HU) reduced platelet accumulation and fibrin deposition following laser-induced injury. Given these results, we tested the hypothesis that IQ would be relatively safe and reduce thrombo-inflammatory biomarkers in steady state SCD patients.
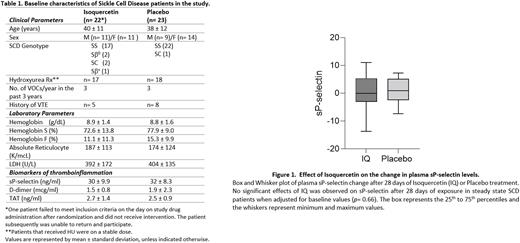
Methods: We conducted a phase II randomized, double blind, placebo-controlled study at the NIH Clinical Center. Eligible patients had SCD, were 60 days remote from an acute VOC or blood transfusion and were on a stable dose of HU. Study subjects (n=46) were randomly allocated to receive either Isoquercetin 1000 mg daily (n= 23) or placebo (n= 23) for 28 days and were monitored at the beginning and at completion of study. The primary endpoint of the study was the ELISA measured change in plasma sP-selectin levels after 28 days of placebo or study drug exposure. Analysis was performed on an intention to treat principle. D-dimer levels and Thrombin anti-thrombin (TAT) complex were measured by Immunoturbidimetric assays and ELISA. Statistical analyses was performed using analysis of covariance (ANCOVA) and Wilcoxon rank-sum test.
Results: The mean (± SD) age of the study population was 40 years (± 11.57), and 56% were female. The majority had HbSS disease and were receiving HU therapy. A subset (28%) reported a prior history of venous thrombosis (VTE) and four of these were on extended duration oral anticoagulation (Table 1). Baseline characteristics between the two study groups were relatively similar. For the primary endpoint, at the end of study the effect of IQ on the change in plasma sP-selectin levels after adjusting for the baseline was not significant (Figure 1) (IQ mean change= 0.10 ± 6.53 vs. placebo mean change= 0.74 ± 4.54; p= 0.66). Since treatment with HU could confound a treatment effect of IQ in a small sample, we compared the change of sP-selectin among those receiving and not receiving HU but did not find any significant difference (p= 0.67). In a sensitivity analysis we did not find an interaction between HU and IQ treatment (p= 0.48). A similar examination for the potential role of VTE history (n= 5 in IQ and n= 8 in placebo arm) as a confounder did not show a VTE effect on change in sP-selectin (p= 0.68) nor an interaction between VTE history and treatment (p= 0.65).
In addition to the primary outcome, we explored the effect of IQ treatment on traditional biomarkers of thrombosis. In contrast to studies in patients with cancer, IQ exposure for 28 days did not have a noticeable effect on change from baseline in either D-dimer levels (IQ mean change= 0.15 mcg/ml ± 0.92 vs. placebo mean change= -0.10 mcg/ml ± 2.11; p= 0.82) or thrombin-antithrombin (TAT) complexes (IQ mean change= 0.09 ng/ml ± 1.60 vs. placebo mean change= -0.05 ng/ml ±1.29; p= 0.57).
Conclusion: Short term Isoquercetin exposure in steady state SCD did not appreciably lower plasma sP-selectin but was well tolerated, safe and did not have bleeding side effects. Clinical studies of higher dose IQ with greater exposure duration may yield more measurable effects on antithrombotic activity.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.